Introduction
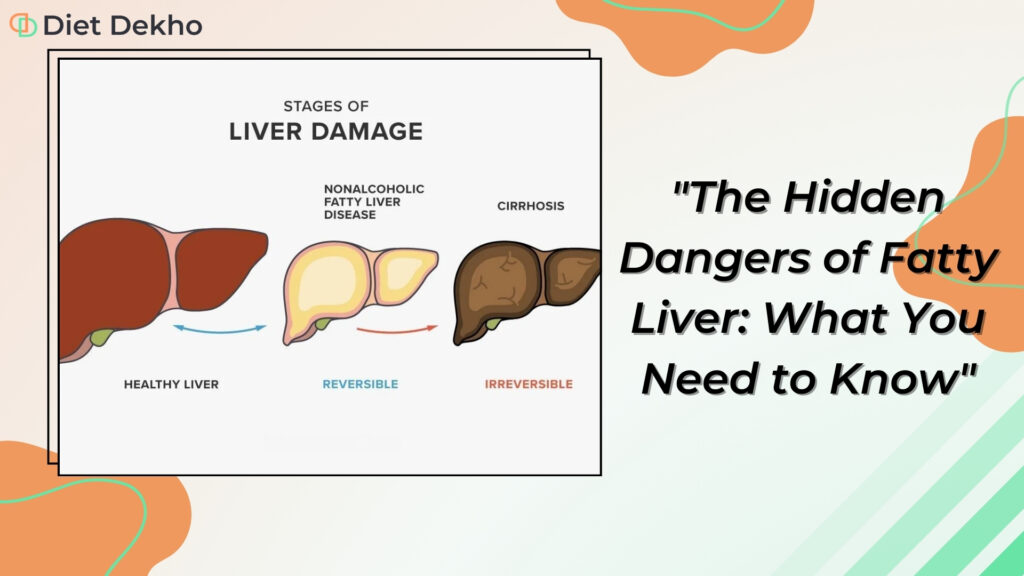
Fatty Liver is a fat disorder that involves abnormal retention of lipids inside the cells in the liver. In our previous blog, we covered the basics of fatty liver disease. We explained its types: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). NAFLD is a condition most seen in people who consume little or no alcohol. NAFLD is linked to many metabolic diseases. These include obesity, type 2 diabetes, and high cholesterol. On the other hand, AFLD is most commonly caused by the overconsumption of alcohol.
The fatty liver may stay symptom-free at first. But, it becomes hard to manage it when it advances to higher, more severe grades. These grades come with serious life implications. This blog explores the hidden dangers of fatty liver. It focuses on the possible complications, risks, and recent research advances on managing it.
Hidden Dangers of Fatty Liver
In its early stages, fatty liver is an asymptomatic disease. Subtle progression may involve grave and treacherous complications due to this condition. The hidden dangers concerning all these should be known so that preventive and treatment measures can be taken.
1.Progression to Serious Hepatic Conditions:
As simple steatosis progresses to NASH, the risk of inflammation and liver cell damage increases. Inflammation can cause fibrogenesis. It leads to scar tissue replacing healthy tissue in the attacked organ. Cirrhosis is due to massive scarring of the liver. It results from heavy fibrotic destruction, which causes liver failure. Cirrhosis greatly raises the risk of liver failure. This life-threatening condition prevents the liver from performing its vital functions.
Cirrhosis causes a lot of scarring. It disrupts the liver’s structure and functions. Plus, it increases infections. Consider these complications, they harm patients’ quality of life. The medical interventions to fix them are often difficult. The link from simple steatosis to cirrhosis shows why we must diagnose and treat fatty liver diseases early.
2. Risk of Liver Cancer:
Chronic inflammation and scarring in the liver promote liver cancers. This is especially true for Hepatocellular carcinoma (HCC), the most common primary liver cancer. Patients with advanced stages of NAFLD or NASH have a higher risk for HCC. Early diagnosis is key to managing this risk. There is research on advanced imaging and biomarkers. They may help diagnose liver cancer earlier in patients with fatty liver disease.
HCC is usually detected late in the course of the disease, and thus it is difficult to treat. Therefore, surveillance in high-risk populations, in particular, those with cirrhosis, is important. The development of non-invasive biomarkers and imaging techniques could help. It could improve the early detection and treatment of liver cancer. This may improve the outcomes for affected individuals.
3. Cardiovascular Complications
Fatty liver disease is closely related to metabolic syndrome. In which hypertension, high blood sugar, and abnormal levels of cholesterol are observed. These pathologies raise the risk of cardiovascular diseases, like heart attacks and strokes. Lipid buildup in the liver affects heart health. So, we must improve the conditions of both the liver and heart in patients.
Common risk factors for NAFLD include obesity, insulin resistance, and dyslipidemia. They increase the risk of cardiovascular events.
4. Type 2 Diabetes and Insulin Resistance
Insulin resistance has been often found to occur with fatty liver disease, where cells tend to become less sensitive to insulin. This will then evolve into type 2 diabetes, further complicating the case of fatty liver disease. In such patients, there exists an added risk of complications. These can be managed by controlling blood sugar levels and maintaining a healthy lifestyle.
Insulin resistance enhances hepatic steatosis through the synthesis of fatty acids from nonlipid sources and reduced lipid oxidation. This metabolic dysfunction worsens liver inflammation and fibrosis. It promotes fatty liver disease. Managing insulin resistance and blood sugar is key to reducing these risks.
5. Impaired Quality of Life
Symptoms and complications of fatty liver disease can produce a significant reduction in quality of life. Fatigue, abdominal pain, and other symptoms, greatly reduce quality of life and daily activities. As the disease advances, the toll may become very burdensome. Effective management strategies may improve life quality. They include lifestyle changes and medical treatments to control common symptoms.
Advanced liver disease often causes hepatic encephalopathy, muscle wasting, and deep fatigue. A multidisciplinary approach can help. It should weaken symptoms via nutrition, physical therapy, and counseling. This can improve patients’ quality of life and function.
6. Economic Burden
The costs of diagnosing and treating fatty liver disease are high. End-stage liver disease is very costly. So are its medications, hospitalizations, and long-term management. It burdens both patients and the health care system. Early detection and prompt interventions are key. They greatly reduce the costs.
Its economic cost can be reduced by preventive measures. These include public health campaigns, lifestyle changes, and early screening programs. Investing in some preventive measures and patient education may reduce advanced liver diseases.
Special Considerations
Fatty Liver in Pregnancy
Acute fatty liver in pregnancy, or AFLP, is a rare but severe condition. It can cause acute liver failure and harm both, the mother and baby. As a result, early diagnosis and proper management are very important for the prevention of such outcomes. A pregnant woman experiencing such symptoms as nausea, vomiting, and abdominal pain should go to the hospital as soon as possible.
AFLP normally occurs in the third trimester and can be extremely critical, at times, even fatal. Other pregnancy-related issues can sometimes suppress its symptoms. This makes it hard to diagnose. Early diagnosis, as part of routine care before birth, can improve recovery. Early intervention, which includes delivering the baby, is key.
Steatosis Hepatis in Adolescence
Pediatric non-alcoholic fatty liver disease (NAFLD) is rising. So is childhood and adolescent obesity. This shows the need for early diet and exercise interventions to prevent liver disease from progressing in this young age group.
In children, it develops silently, but it can be easily detected with periodic health check-ups by liver enzyme elevations. We should encourage children to eat healthy, exercise, and maintain a healthy weight. This can help reverse fatty liver and prevent long-term liver damage. Early diagnosis and management of NAFLD in pediatric years can help to reverse the process aptly and save the liver from any further damage. Pediatricians have a pivotal role to play in early diagnosing and managing NAFLD in these young patients.
Diabetic and Fatty Liver
Diabetes and fatty liver often coexist together and have a bidirectional complex relationship, aggravating both. Appropriate control of blood sugar, through medication, diet, and exercise, is important for patients with co-existing disease to prevent further deterioration of liver disease and other complications.
A person who has both diabetes and fatty liver has an even more increased risk of having NASH and liver fibrosis. Proper management includes monitoring liver function regularly in order to optimize the treatment for glycemic control and other metabolic risk factors like hypertension and dyslipidemia. The management approach for such patients should be effective and should always keep in mind that such patients require collaboration between the endocrinologist and hepatologist.
Metabolic Fatty Liver Syndrome
Fatty liver disease is closely linked to metabolic syndrome. This is a mix of obesity, insulin resistance, high blood pressure, and bad cholesterol. Lifestyle changes and medications can alter these metabolic syndrome components. They can also prevent and reduce fat in the liver.
Lifestyle changes are key to treating metabolic syndrome. These include a low-calorie diet and exercise. Blood pressure, lipid profile, and blood sugar need to be controlled if insane, and medications may be needed. Promptly spotting and treating liver disease in those with metabolic syndrome could change its course for the good
Pediatric Non-Alcoholic Fatty Liver Disease.
NAFLD in children and adolescents will slowly advance to more advanced liver disease in later adult life. It is vital to stop disease progression in kids. A healthy diet and enough exercise can do this. They are key in preventing liver disease.
Most children with NAFLD are obese. Family-based lifestyle changes could treat this. They could help with weight management. The schools and community can also help in promoting healthy behaviors among the children. Regular follow-ups with pediatric NAFLD are needed. They must include serial assessments to prevent advanced liver disease.
Conclusion
Many hidden dangers are associated with fatty liver diseases, such as progression to serious hepatic conditions, increased risk of liver cancer, cardiovascular complications, and type 2 diabetes; besides impaired quality of life and economic burden. Early diagnosis of these diseases, followed by the introduction of lifestyle changes and appropriate medical interventions, is of great importance for management and prevention. By understanding and addressing these hidden dangers, we may reduce complications and improve health outcomes and quality of life for patients with fatty liver disease.