Have you ever felt a heavy, persistent fatigue that a full night’s sleep just won’t touch? Perhaps you’ve noticed that despite hitting the gym and skipping the obvious sweets, the weight around your waistline refuses to budge. Many people feel like they are fighting a losing battle with their own biology, and honestly, they usually are. What this really means is that your body might be struggling with a silent metabolic shift. If you are searching for the best diet for insulin resistance, you aren’t just looking for a meal plan; you are looking for a physiological reset button.
Table of Contents
- 1 The Biological “Lock and Key” Mechanism
- 2 Why Evolution Saved This “Faulty” Logic
- 3 Recognizing the Silent Signals of Resistance
- 4 The Alarming Global Metabolic Crisis
- 5 Choosing Your Metabolic Shield: The Mediterranean Diet
- 6 The DASH Diet: More Than Just Blood Pressure
- 7 Managing the “Carb Curve”: Glycemic Index vs. Load
- 8 The High-Fiber Advantage
- 9 The 10-Minute Metabolic Secret
- 10 Surprising Kitchen Allies: Lemon Juice and Vinegar
- 11 The Silent Threat of Sleep Deprivation
- 12 Your Roadmap to Reversing the Damage
- 13 Sample 7-Day Metabolic Reset Meal Plan
- 14 Frequently Asked Questions
The Biological “Lock and Key” Mechanism
Let’s break it down simply. Your body uses a hormone called insulin to ferry sugar (glucose) out of your blood and into your cells for energy. Think of insulin as a key and your cells as a door. When you have insulin resistance, the lock gets jammed. Because the “door” won’t open, sugar stays stuck in your bloodstream, and your pancreas works overtime to pump out even more insulin to compensate. This creates a vicious cycle called hyperinsulinemia.
Surprisingly, recent research from Harvard Medical School shows this problem goes much deeper than just the cell surface. Scientists found that the insulin receptor actually relocates to the cell nucleus to control gene expression. In cases of resistance, there is a staggering 30-fold reduction in this process. This genetic impairment effectively disrupts how your body handles fat and energy at a foundational level.
Why Evolution Saved This “Faulty” Logic
You might wonder why our bodies would even allow such a damaging process to exist. Actually, insulin resistance likely served as an evolutionary survival tool. During periods of starvation, the body breaks down stored fat, which temporarily makes muscle and liver cells resistant to insulin. This process preserves precious blood sugar for the brain to ensure survival.
The trouble starts because we now live in a world of constant fuel overload. Our modern diet of refined carbs and saturated fats keeps this “starvation mode” perpetually switched on. Instead of protecting us from famine, this mechanism now drives chronic disease by storing fat in places it shouldn’t be, like your liver and muscles.
Recognizing the Silent Signals of Resistance
Insulin resistance often develops quietly without any obvious symptoms for years. However, the body does leave clues if you know where to look. Experts suggest the most reliable “moment of truth” involves a simple tape measure at home. If your waist size measures over 35 inches for women or 40 inches for men, your risk for metabolic syndrome increases significantly.
| Clinical Marker | Risk Threshold | Why It Matters |
| Waist (Men) | ≥40 inches | Indicates visceral fat |
| Waist (Women) | ≥35 inches | Links to metabolic syndrome |
| Triglycerides | ≥150 mg/dL | Shows unhealthy blood fats |
| HDL (Good) | <40−50 mg/dL | Lowers heart protection |
| Blood Pressure | ≥130/85 mmHg | Suggests vascular stress |
| Fasting Glucose | 100−125 mg/dL | Marks the prediabetes range |
The Alarming Global Metabolic Crisis
What this really means for our health is quite sobering. According to systematic reviews of over 235,000 participants, the global prevalence of insulin resistance has hit roughly 26.5%. Essentially, one in four adults is currently struggling with some level of metabolic impairment. Even more concerning, 2024 data from the UK links insulin resistance to over 30 different diseases, including Parkinson’s and pancreatitis.
For women, the stakes are even higher. Every one-unit increase in insulin resistance scores correlates with an 11% higher risk of early death. Since high insulin acts as a rogue agent promoting inflammation and abnormal cell growth, it even acts as a fuel for certain cancers. This is why finding the right eating strategy isn’t just about weight—it’s about long-term survival.

Choosing Your Metabolic Shield: The Mediterranean Diet
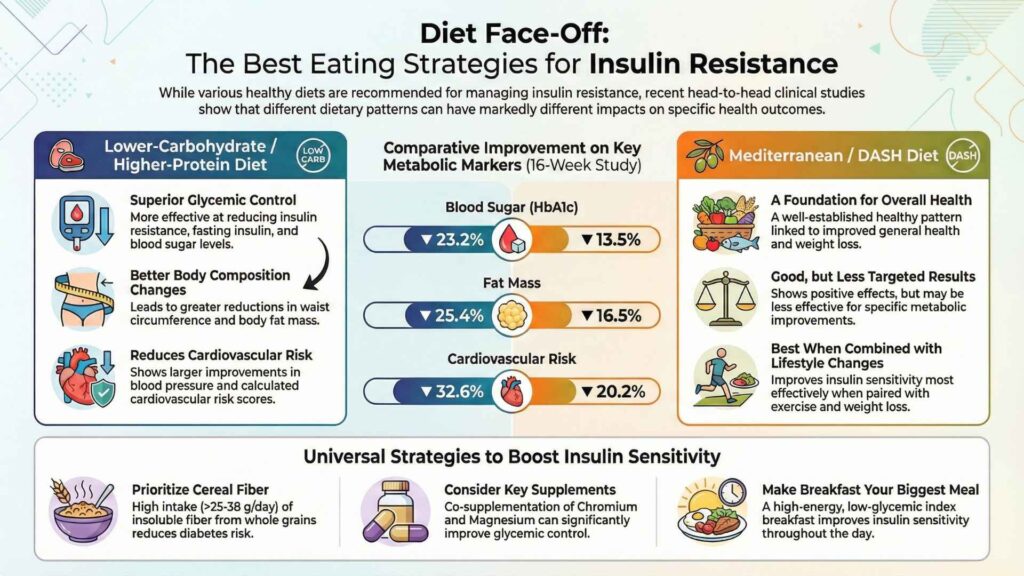
When it comes to the best diet for insulin resistance, the Mediterranean pattern consistently takes the gold medal. This eating style focuses on anti-inflammatory whole foods like extra-virgin olive oil, legumes, leafy greens, and fatty fish. Because it emphasizes healthy fats over refined carbs, it helps stabilize the insulin response naturally.
Healthy fats, like the monounsaturated fats found in olive oil and avocados, actually increase a hormone called adiponectin. This hormone directly improves your insulin sensitivity and calms systemic inflammation. Unlike traditional low-fat diets that often swap fat for sugary “diet” foods, the Mediterranean approach keeps you full and metabolically stable.
The DASH Diet: More Than Just Blood Pressure
If you also struggle with high blood pressure, the DASH (Dietary Approaches to Stop Hypertension) diet offers a powerful alternative. While doctors originally designed it for heart health, DASH has proven highly effective at improving insulin resistance and obesity. The plan prioritizes potassium, calcium, and magnesium—minerals that are vital for proper glucose metabolism.
| Food Group | DASH Daily Goals | Mediterranean Focus |
| Vegetables | 4–5 servings | High variety & unlimited |
| Whole Grains | 6–8 servings | Unrefined/Ancient grains |
| Lean Protein | ≤6 oz daily | Focus on fatty fish/legumes |
| Healthy Fats | 2–3 servings | Primary source: Olive oil |
| Dairy | 2–3 servings | Fermented (Yogurt/Kefir) |
Managing the “Carb Curve”: Glycemic Index vs. Load
Let’s clear up the confusion about carbohydrates. Many people think they have to quit all carbs to fix insulin resistance, but that isn’t true. What matters most is the “Glycemic Index” (GI), which ranks how fast a food spikes your blood sugar. Low-GI foods (score of 55 or less) digest slowly, providing a steady stream of energy rather than a massive insulin surge.
However, the Glycemic Load (GL) is an even better tool. While GI tells you how fast blood sugar rises, GL tells you how much sugar is actually in a serving. For example, watermelon has a high GI but a low GL because it’s mostly water. Focusing on a low-GL diet is significantly more effective for metabolic health than just cutting fat.

The High-Fiber Advantage
If you want a “metabolic hack,” look no further than fiber. Experts recommend aiming for up to 50 grams of fiber per day to maximize insulin sensitivity. Fiber acts like a physical shield in your gut, slowing down the absorption of sugar and preventing the spikes that drive resistance.
Excellent sources include chia seeds, flaxseeds, beans, and non-starchy vegetables. Beyond blood sugar, fiber also feeds your gut microbiome, which produces short-chain fatty acids that further reduce inflammation. It’s essentially the simplest way to “blunt” the impact of the carbs you do eat.
The 10-Minute Metabolic Secret
Here is the thing: you don’t need a grueling 2-hour gym session to see results. A Harvard-trained specialist recently highlighted that a simple 10-minute walk after meals can be a game-changer. When your leg muscles move after eating, they draw glucose directly from your bloodstream for fuel without needing much insulin.
This habit reduces insulin spikes and helps prevent fat from being stored in your liver. Whether you are walking around your living room or taking a stroll outside, the consistency of moving after you eat can be as effective as some medications. It is an accessible, free tool for anyone looking to reclaim their health.
Surprising Kitchen Allies: Lemon Juice and Vinegar
But wait, there’s more you can do in the kitchen. Scientific research now reflects what holistic healers have said for years: acidic foods like lemon juice and vinegar can lower the glycemic response of your meal. Experts suggest that adding lemon juice to your water or vinegar to your salad dressings slows the rate at which your stomach empties.
This slower digestion leads to improved insulin sensitivity and more stable blood sugar levels. In fact, some clinical programs have used lemon juice as a core strategy for over a decade to facilitate detoxification and metabolic reversal. It’s a small, intentional choice that yields real biological benefits.

The Silent Threat of Sleep Deprivation
We often overlook it, but sleep is a non-negotiable pillar of metabolic health. Research shows that even a single night of poor sleep can spike your insulin resistance levels the next day. When you are sleep-deprived, your body produces more cortisol, which tells your liver to dump glucose into your blood.
Aim for 7 to 9 hours of quality rest every night. To help your body stay sensitive to insulin, try to “close the kitchen” a few hours before bed. Late-night eating is closely linked to higher resistance levels, as the body isn’t primed to handle a sugar load while you are sleeping.
Your Roadmap to Reversing the Damage
The most important takeaway is this: insulin resistance is not a life sentence. Unlike Type 1 diabetes, you can often reverse this condition through targeted lifestyle shifts. Losing just 5% to 10% of your body weight can clear out the “ectopic” fat stored in your liver and pancreas, allowing them to function normally again.
Personalized guidance makes this journey much easier. Programs like those at(https://dietdekho.com/form/) provide the structure you need, offering customized plans that have already impacted over 19,600 lives. With a 98% success rate, their expert coaches take the mystery out of grocery shopping and meal timing, ensuring you stay on track for a total metabolic reset.
Sample 7-Day Metabolic Reset Meal Plan
This framework prioritizes high-fiber, low-GI foods to keep your insulin levels low and your energy high.
- Monday: Breakfast: Greek yogurt with chia seeds and blueberries. Lunch: Grilled chicken salad with avocado. Dinner: Baked salmon with roasted broccoli and quinoa.
- Tuesday: Breakfast: Scrambled eggs with spinach and tomatoes. Lunch: Turkey and avocado lettuce wraps. Dinner: Stir-fried tofu with zucchini over cauliflower rice.
- Wednesday: Breakfast: Steel-cut oats with flaxseeds and raspberries. Lunch: Lentil soup with an arugula salad. Dinner: Grilled shrimp with asparagus and lemon.
- Thursday: Breakfast: Spinach omelet with avocado. Lunch: Tuna salad with mixed greens and cucumber. Dinner: Turkey meatballs with zucchini noodles.
- Friday: Breakfast: Smoothie with spinach, protein powder, and berries. Lunch: Chickpea and quinoa salad. Dinner: Baked cod with sautéed kale and lentils.
- Saturday: Breakfast: Almond flour protein pancakes with berries. Lunch: Veggie frittata. Dinner: Chicken stir-fry with bell peppers and cabbage.
- Sunday: Breakfast: Low-carb breakfast burrito with black beans and eggs. Lunch: Caprese salad with fresh mozzarella. Dinner: Herb-roasted pork with green beans.

Frequently Asked Questions
What are the best low glycemic index foods to include in my diet? You should focus on non-starchy vegetables (like kale and broccoli), berries, beans, lentils, and intact whole grains like steel-cut oats. These foods digest slowly and prevent the massive blood sugar spikes that worsen resistance.
How can I naturally improve my insulin sensitivity? The best way involves a combination of high-fiber eating, regular post-meal walks, 7-9 hours of sleep, and stress management. Each of these habits helps lower cortisol and allows your cells to respond better to insulin.
Can a meal plan for insulin resistance help with weight loss? Absolutely. High insulin is a fat-storage hormone. By following a plan that lowers insulin levels, you allow your body to access and burn stored fat more effectively, which naturally leads to weight loss.
What is the difference between glycemic index and glycemic load? Glycemic index (GI) measures how fast a food raises blood sugar, while glycemic load (GL) accounts for the actual amount of carbs in a serving. GL is generally a more accurate way to predict how a specific portion will affect your levels.
Is it possible to reverse insulin resistance through diet alone? Diet is the most powerful lever, but it works best when paired with movement. Studies show that losing as little as 5-7% of your body weight through diet and activity can significantly reduce your risk of metabolic disease.
Metabolic health isn’t about being perfect; it’s about being intentional. By choosing nutrient-dense foods and moving your body, you can break the cycle of fatigue and weight gain once and for all. If you are ready for a personalized plan tailored to your unique biology, connect with the experts at(https://dietdekho.com/form/) today to start your journey.
BOOK YOUR APPOINTMENTAbhinav is the Founder of Diet Dekho, helping people manage weight and lifestyle health through simple, practical nutrition and personalized diet plans.
